Chronic Pancreatitis:
Severe recurrent upper abdominal pain is the most common and prominent symptom of chronic pancreatitis patients. Therefore, pain relief and improvement in patients’ quality of life are the primary goals in the treatment of this disease. As a first approach, patients should be managed conservatively. If medical treatment fails, endoscopic intervention can offer pain relief in the majority of patients in the short term. However, recent data suggests that - at least in complex disease - surgical treatment is superior to endoscopic intervention since it provides superior long-term results. Several surgical drainage procedures and resection techniques have been introduced and proven to be effective. However, the duodenum preserving surgical techniques should be favored, since they are safer and even more efficient than the classical Whipple’s procedure. They have shown to offer adequate pain control and improvement in quality of life in most patients. At the same time they can be performed with low morbidity and mortality rates, preserving endocrine and exocrine function of the pancreas and therefore ensuring an improvement of patients’ quality of life.
1. Introduction
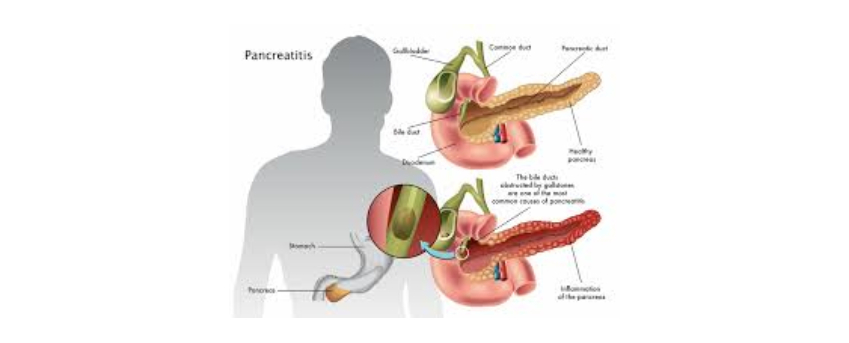
Chronic pancreatitis (CP) is a benign inflammatory disease that leads to progressive and irreparable destruction of the pancreatic parenchyma, resulting in fibrosis and consequent loss of exocrine and endocrine function (14, 46). This may cause steatorrhea, malabsorption, diabetes and unbearable pain (52). Pain - often in combination with obstruction (duodenum, bile duct, pancreatic duct, portal vein) - remains the main indication for surgical intervention.
The incidence of CP varies between countries. European studies commonly show incidence rates around 7 per 100,000 (16, 33, 42) while higher incidence rates of 14.4 per 100,000 have been reported for example in Japan (40). The leading cause of CP in Western industrialized countries is alcohol over-consumption (between 65% and 90%) followed by idiopathic (20–25%) and other rare etiologies (5%) (16, 33, 40).
Patients typically present with deeply penetrating and dull epigastric pain, which classically radiates to the back (32). The pathophysiological mechanisms for pain in CP are incompletely understood. An increasingly discussed hypothesis is that neural inflammatory cell infiltration leads to pancreatic neuritis with enlarged nerves, changes in neural plasticity, and formation of a dense intrapancreatic neural network. These neural alterations are thought to cause the characteristic pancreatic neuropathy and consequent neuropathic pain (7-11). Since the underlying pain mechanisms are just beginning to be understood, treatment of chronic unbearable CP pain is often empirical and insufficient, with surgery remaining the treatment of choice.
2. Indication for surgery: wait, operate or scope?
Making the correct diagnosis is the initial challenge in the treatment of painful CP, which can be difficult, especially in patients with early forms of CP, lacking the structural changes frequently seen in advanced disease. Most patients require long-term analgesic medications for pain control once the diagnosis is confirmed. Moreover, patients should be advised to maintain strict abstinence from alcohol and tobacco. Pain medication should be employed according to the step up approach of the WHO analgesic ladder. Despite low evidence for efficacy in pancreatic pain, non-narcotic adjunctive medications like selective serotonin reuptake inhibitors (SSRIs) or pregabalin have become increasingly popular in CP treatment, since these agents were proven effective in other chronic pain states (21, 36). Pancreatic enzyme supplementation is also used, although evidence concerning pain reduction is conflicting (3, 26, 35, 37, 49, 51). If medical therapy proves insufficient, and there is no sign of pancreatic or biliary duct obstruction, more invasive non-operative strategies like coeliac nerve block may be considered. EUS-guided techniques have in this context proven safer, more effective, and longer lasting than fluoroscopy-guided or CT-guided techniques (29, 44, 45). However, coeliac nerve block usually generates a transient effect, with only 10% of patients still experiencing pain relief after 24 weeks (25). Therefore, this option seems more reasonable in patients with malignant disease and a anticipated short life span.
In patients with CP and obstruction of the pancreatic duct, endoscopic treatment for ductal decompression including papillotomy, stone removal, and/or stent implantation is another widely used treatment option. Classical indications for surgery in CP are pancreatic duct obstruction, vascular obstruction, suspicion of neoplasm, and abdominal pain with failure of conservative treatment options. So far, only two prospective randomized clinical trials addressed the question whether endoscopic or surgical drainage is superior to treat symptomatic pancreatic duct obstruction. Dite and colleagues were the first to address this controversial issue in a randomized controlled trial, where 72 patients were randomized to surgery vs. endoscopy (15). Resection was the most common surgical procedure (80%) while surgical drainage was performed in 20% of patients. On the other hand, sphincterotomy and stenting (52%) and/or stone removal in 23% of patients were the most commonly performed intervention in the endoscopy arm. While the initial success rates for pain relief were similarly high (> 90% of patients with at least a partial pain relief after 1 year follow up) for both groups, these clinical outcomes changed noticeably after 3 and 5 years follow up. In the surgical treatment group 42% of patients showed a persistent complete pain relief after 1 year, which only slightly decreased to 41% after 3 and to 37% after 5 years. Initially, an equally good clinical outcome was seen in patients in the endoscopic treatment arm where 52% of patients showed a complete pain relief after 1 year. But this effect substantially decreased to 11% after 3, and to 14% after 5 years. Accordingly, the rate of non-responders was disappointingly high with 33-35% in the endoscopy arm versus only 12-14% in the surgical treatment arm after 3 and 5 years. Results were similar regarding the patient’s body weight. Therefore, Dite and colleagues concluded that surgery seems to be superior to endoscopic treatment concerning long-term pain relief and body weight gain in CP patients. It should be noted however, that endoscopic drainage techniques in this study did not meet current standards as it did not include ESWL (extracorporeal shockwave lithotripsy) and for some patients only consisted of a sphincterotomy.
In 2007, Cahen and colleagues published the second randomized trial on this subject (6), which was updated with long-term outcomes in 2011 (5). In this trial, 39 patients were randomized between endoscopic (n=19) and surgical drainage by a pancreaticojejunostomy (n=20). The study was preterminated following an unscheduled interim analysis after a median of 24 months, because of a highly significant difference in the mean Izbicki pain score (11 vs. 34) favoring the surgical treatment arm (p<0.001). Even more striking were the vast differences in frequency of patients with complete or partial pain relief at the end of the first follow-up, with only 32% of patients in the endoscopic treatment group but 75% in the surgical treatment group showing at least partial pain relief. Furthermore, at long-term follow up of up to 7 years, these numbers did not change considerably (38% vs. 80%). Additionally, endoscopically treated patients underwent significantly more re-interventions than surgically treated patients (8 vs. 3 at first follow up and 12 vs. 4 at the second follow up). Based on these results, the authors concluded that surgical drainage is superior to endoscopic treatment and should be regarded as the preferred treatment option in patients with advanced disease.
Based on these two randomized trials it can be concluded that surgical therapy is more effective and longer lasting than endoscopic treatment. There may be a role for endoscopic drainage early in the disease course. However, surgical treatment for pain in CP should also be considered early in disease history especially in patients with pancreatic calcifications. Current data on the optimal timing of surgical intervention is not sufficient to make final recommendations. Nealon and colleagues suggested that early operative duct decompression may delay progressive functional destruction of the pancreas (39). While similar conclusions were drawn from Ihse et al. (27), others have described a progressive functional impairment despite surgery (50), meaning that to date, the question of optimal timing of surgery remains unclear. From the study from Cahen and colleagues we know that the large group of patients that were secondarily operated after endoscopic failure (47%) also did not do well after surgery (6). This suggests that early intervention may to be a key factor for success in the treatment of CP irrespective of the type of intervention. Current guidelines suggest that if endoscopic therapy is insufficiently effective after one year, the patient should be referred to surgery.
3. Surgical options: how to operate – drain or resect?
Two main forms of surgical interventions are presently performed for CP patients with the aim of improved drainage of the pancreatic duct: drainage and resection procedures. Any of these surgical interventions should be aiming to relieve pain while at the same time preserving as much of the pancreatic parenchyma and being as safe as possible. In the early 19th century the first surgical attempts to relieve pancreatic pain in CP aimed at draining the pancreatic duct by means of pancreatostomy (34) or pancreatic left resection (17). Surgical strategies for the treatment of chronic pancreatitis have continuously evolved since then. Puestow and Gillesby were the first to present a modification with combined pancreatic left resection, longitudinal opening of the pancreatic duct and an anastomosis to the small intestine (pancreaticojejunostomy) (43). In 1960, Partington and Rochelle published what they called the modified Puestrow-Gilles procedure: a spleen-preserving longitudinal pancreaticojejunostomy, where they preserved the tail of the pancreas and extended the opening of the pancreatic duct (41). This surgical technique is nowadays known as the Partington-Rochelle procedure and represents the favored surgical drainage procedure for treatment of CP for many years. These draining procedures preserve a maximum of pancreatic tissue; however the major disadvantage of these procedures is that the frequently associated inflammatory mass in the pancreatic head and therefore the underlying cause of the disease is not addressed. Nowadays the only suitable indication for a simple drainage procedure and for longitudinal pancreaticojejunostomy is in patients with isolated pancreatic duct pathology (dilated duct of > 7mm; ‘chain of lakes’), without an inflammatory mass in the pancreatic head. For the select group of patients, long term pain relief of this drainage operation has been shown to be around 60-70%, and up to 98% with low mortality and morbidity (approximately 3% and 20%, respectively) (23, 24).
Pain in patients without pancreatic duct dilation is thought to evolve from neuropathic changes within the pancreatic head, as described earlier. The pancreatic head has been identified as the derivation of the disease, long before these underlying neural alterations were discovered (2). Therefore, several surgical techniques have been implemented for the resection of the pancreatic head within the last century. The first resection of the pancreatic head was performed 1909 in Berlin by Walther Carl Eduard Kausch on a patient with periampullary cancer. It was the introduction of a technique, nowadays known as the standard Kausch-Whipple procedure, which encompasses the radical resection of the pancreatic head, the duodenum, the gastric antrum with the pylorus and the gallbladder. While it was initially established for the treatment of malignancies, it was later also used for the resection of inflammatory pancreatic head masses. Due to relatively high rates of gastrointestinal complications and diabetes mellitus, the classic Kausch-Whipple procedure has been replaced by the pylorus preserving Whipple procedure, introduced by Traverso and Longmire in 1978 (19, 48). This Traverso-Longmire procedure has been shown to lead to long-term pain relief in around 90% of patients with painful chronic pancreatitis (19, 38).
In the early 1970s, Beger introduced the duodenum preserving pancreatic head resection (DPPHR), with the rationale that resection of the gastric antrum, duodenum and common bile duct seemed overtreatment in benign pancreatic disease (1). For the Beger procedure, a subtotal resection of the pancreatic head prior to a transsection of the gland above the portal vein is performed, sparing the duodenum and the intrapancreatic bile duct. The drainage of the remaining pancreatic tail is then achieved by an end-to-end or end-to-side pancreaticojejunostomy using a Roux-en-Y loop.
Frey et al modified the established procedures to a more limited and organ-preserving resection,which is performed by coring out the head of the pancreas and leaving a small remnant along the duodenal wall (20). Frey and colleagues then combined this procedure with a longitudinal incision of the left-sided main pancreatic duct for optimal drainage, comparable to the earlier mentioned Partington–Rochelle drainage procedure. For reconstruction, a longitudinal pancreaticojejunostomy using a Roux-en-Y loop is used for drainage of the pancreatic head cavity and the left-sided main duct. The Frey procedure is commonly regarded as technically easier than the Beger operation, as the head resection is more limited, dissection of the pancreas above the portal vein is not required, and the reconstruction is less complex.
At last, the Beger technique of DPPHR has been further modified and described by Gloor et in 2001, often referred to as the Bern procedure (22). The idea was to combine advantages of both the Beger and Frey operation. For the Bern procedure, a deep duodenum-preserving resection of the pancreatic head for optimal decompression is performed, without transection of the pancreas above the portal vein. In contrast to the Frey procedure and the Hamburg procedure, no drainage of the main pancreatic duct in the body and tail of the organ is performed. Drainage of the resection cavity of the pancreatic head is achieved as in the Beger procedure, by creating a pancreaticojejunostomy using a Roux-en-Y loop. When it comes to the question as to which of these procedures one should choose, evidence is limited to some monocentric trials (Table 1). Klempa and colleagues have compared the classic Whipple procedure (n=21) with the Beger procedure (n=22) in the first randomized controlled trial on the type of surgical treatment for painful chronic pancreatitis in 1995. Here, patients with a Beger procedure had less pain, a better gain in body weight and a shorter hospital stay (30). A similar study was published by Büchler et al., comparing the duodenum preserving pancreatic head resection (n=20) to the pylorus preserving Whipple procedure (n=20). Again, the duodenum sparring resection had a better outcome in terms of pain, weight gain, glucose tolerance, and insulin secretion capacity (4). Two randomized trials compared the pylorus-preserving Whipple procedure to the Frey procedure, and both showed that these procedures were equally efficient for pain relief, but that the Frey procedure provides better quality of life (18, 28). Strate et al. could not show any difference regarding mortality, quality of life, pain, or exocrine and endocrine function when comparing the Beger procedure (n= 38) to the Frey procedure (n=36) (47). The most recent randomized trial by Köninger et al. has been published in 2008 and shows that the Bern procedure can be performed significantly faster and leads to shorter hospital stay than the Beger operation (31). In 2010, Diener and colleagues published the protocol for the ChroPac Trial, which is the first large randomized controlled multicenter trial comparing duodenum preserving pancreatic head resection vs. pancreatoduodenectomy with the primary outcome being patient’s quality of life 24 months after surgery (12). First results of this trial are expected in late 2016. The current evidence is best summarized in a recently published meta-analysis, where duodenum preserving pancreatic head resections (including Beger, Frey, and Büchler procedures) and pancreatoduodenectomy were shown to be equally effective in terms of pain relief, overall morbidity and incidence of postoperative endocrine insufficiency (13). However, the duodenum preserving pancreatic head resections seems to be superior in terms of postoperative weight gain and long-term quality of life. Similar results were obtained for the Beger and Frey procedures. Therefore, despite the lack of clear multicenter randomized controlled trial evidence, it seems that any of these duodenum preserving resection techniques is appropriate for the surgical treatment of painful chronic pancreatitis and that to date, these should be preferably performed over pancreatoduodenectomy (Whipple operation).
4. Conclusion
Long-term pain relief, resolving complications in pancreas-neighboring organs, and improvements in patient’s pain and quality of life remain the primary goals in treating CP. This should be approached interdisciplinary, by a team of radiologists, pain specialists, gastroenterologists and surgeons. Endoscopic drainage may have a role in early disease. However, if persistent pain reduction and consequent improvement in patient’s quality of life cannot be achieved by conservative therapy within one year, surgery is the treatment of choice which is superior to endoscopic treatment in the long term. Pancreatic resections for CP have low morbidity and mortality rates in high-volume centers and promise long-term pain relief for the vast majority of patients with painful chronic pancreatitis. When it comes to surgical techniques, drainage operations are safe and efficient for short-term pain relief, especially in patients without an enlarged pancreatic head, but often fail in the long-term. The Kausch-Whipple operation has been the standard of care for decades, but was steadily replaced by the pylorus preserving modification from Longmire and Traverso. Persistently high morbidity rates and insufficient long-term effects after these extensive resections have lead to the development of more tissue preserving techniques. Nowadays, the duodenum preserving resection techniques offer the best outcome for patients with painful chronic pancreatitis and an inflammatory mass in the pancreatic head and should therefore be considered as the current standard of care, while the different variants of this technique seem to retrieve similar results (27, 39, 50).